October – synonymous with pumpkin spice everything and the color pink! Yep, it’s Breast Cancer Awareness Month! – probably the most well-known health awareness observation. Thousands of organizations and millions of people come together each year to highlight the importance of breast awareness, education, and research. It’s pretty powerful – and important – since breast cancer continues to be the second most common type of cancer among women in the United States (behind skin cancer) and the second leading cause of cancer death in women. About 1 in every 8 women will be diagnosed with breast cancer at some point during her life.
At the Wisconsin Women’s Health Foundation, we have pink fever too, and we will be sharing helpful breast cancer information with you all month long.
If you haven’t already, subscribe to our blog. You won’t want to miss any of this discussion!
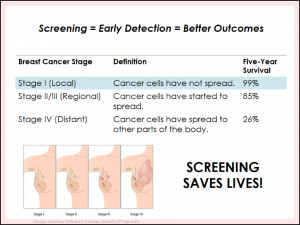
SCREENING SAVES LIVES
When it comes to breast cancer screening recommendations, it can get complicated, but the simple truth is this: screening saves lives! Time and time again, research has shown that screening leads to earlier detection of cancer, and earlier detection means more treatment options and a better chance of survival.
In our FREE GrapeVine health education sessions on breast cancer, we share the following chart from the National Cancer Institute, which shows when breast cancer is caught at an early stage, survival rate is nearly 100%. However, as cancer gets more advanced and starts spreading, the chances of survival greatly decrease.
Screening and identifying a breast problem can be the difference between a potentially curable cancer and a poor outcome!
HOW DO I SCREEN?
There typically have been three common types of screening methods to detect breast cancer:
Breast Self-Exams: when a woman inspects her own breasts to detect any abnormalities
Clinical Breast Exam: when a doctor visually checks for abnormalities of the breast during your regular check-up
Mammogram: X-ray images of the breast to detect subtle changes which may indicate breast cancer
However, it’s important to note that based on research, breast self-exams and clinical breast exams are no longer recommended by many health leaders. The consensus is that mammograms are the gold standard for screening. With that being said, all women should still be familiar with the normal look and feel of their breasts, so they can report any changes to their healthcare provider right away. The bottom line: Know your body. Even though self breast exams are no longer recommended, doing them may help you keep an eye on changes.
For more about the 12 signs of breast cancer, visit Know Your Lemons. And to read about our very own Program Evaluation Manager’s experience with finding a lump, read Emily’s story.