
Cervical Health Awareness Month
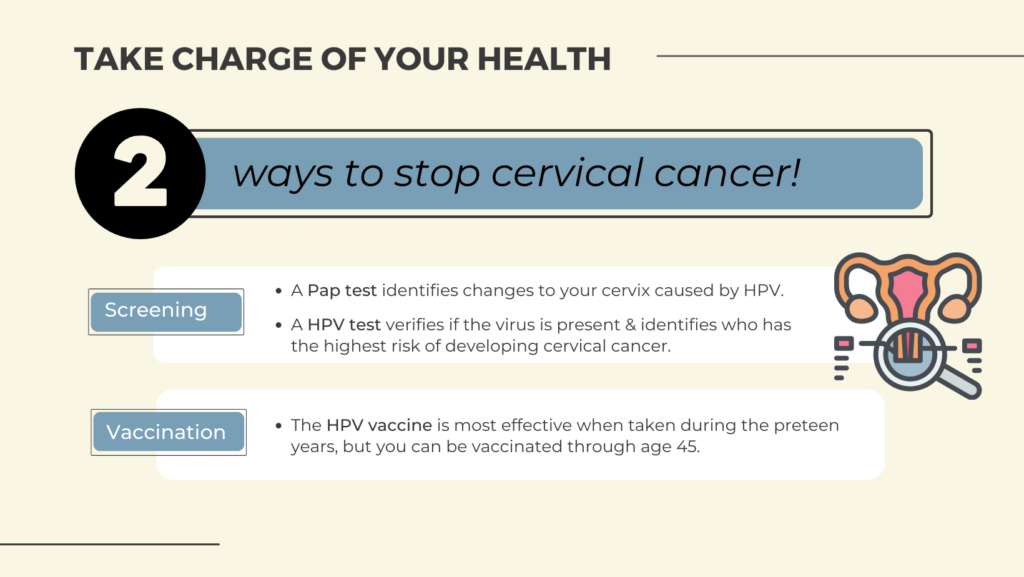
Take Charge of Your Health
January is Cervical Cancer Awareness Month and an important time to educate and advocate for our health. The CDC estimates up to 93% of cervical cancers are preventable with screening and HPV vaccinations.
Talk to your healthcare provider about cervical cancer prevention. You can also learn more about all gynecological cancers, their risk factors and prevention in one of GrapeVine’s health webinar sessions.
What Is Cervical Cancer?
Cervical cancer is cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, if not destroyed or removed, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
Cervical Cancer Causes, Risk Factors, and Prevention
HPV infection causes cervical cancer
Long-lasting (persistent) infection with high-risk types of human papillomavirus (HPV) causes virtually all cervical cancer.
Nearly all people who are sexually active will become infected with HPV at some point in their lives. Around half of HPV infections are with a high-risk (cancer-causing) HPV type. High-risk HPV can cause several other types of cancer as well as cervical cancer. HPV16 and HPV18 are the high-risk types that cause most cases of cervical cancer.
Most HPV infections go away on their own as the immune system controls the infection. When a high-risk HPV infection lasts for many years, it can lead to changes in the cervical cells that, if untreated, can become cancer.
Other factors can increase your risk of cervical cancer
Some risk factors make it more likely for a person who has a high-risk HPV infection of the cervix to have a persistent infection that leads to severe cervical cell changes that can develop into cervical cancer. These risk factors include:

- Having a weakened immune system: This can lower the body’s ability to fight HPV infection and other diseases. HPV infections are more likely to be persistent and progress to cancer in people who are immunocompromised than in people who are not immunocompromised. You may be immunocompromised if you:
- Have HIV infection or another disease that weakens the immune system.
- Take medicine to suppress your immune response, such as to prevent organ rejection after a transplant, to treat an autoimmune disease, or to treat cancer.
- Smoking or breathing in secondhand smoke: Those who either smoke or breathe in secondhand smoke have an increased risk of developing cervical cancer. The risk increases the more a person smokes per day and the longer a person has smoked.
- Becoming sexually active at an early age: The risk of high-risk HPV infection that is persistent and ultimately leads to cervical cancer is higher in people who become sexually active before age 18 and in those who have had multiple sexual partners. This sexual history increases the chances of exposure to high-risk HPV.
- Other reproductive factors: Both the use of oral contraceptives (birth control pills) and giving birth to many children have been found to be associated with cervical cancer risk. The reasons for these associations are not well understood.
DES exposure is a rare cause of cervical cancer
Being exposed to a drug called diethylstilbestrol (DES) in the womb is an independent risk factor for a type of cervical cancer called clear cell adenocarcinoma. Between 1940 and 1971, DES was given to some pregnant women in the United States to prevent miscarriage (premature birth of a fetus that cannot survive) and premature labor. Women whose mothers took DES while pregnant have an increased risk of cervical cell abnormalities and of clear cell adenocarcinoma of the vagina and cervix.
Cervical cancer is preventable
Cervical cancer is highly preventable and highly curable if caught early. Nearly all cervical cancers could be prevented by HPV vaccination, routine cervical cancer screening, and appropriate follow-up treatment when needed.
HPV vaccination
HPV vaccination is a safe and effective way to help prevent cervical cancer. Gardasil 9 is the FDA-approved vaccine for females and males aged 9 to 45 years in the United States. Gardasil 9 is nearly 100% effective in preventing cancer caused by all seven cancer-causing HPV types (16, 18, 31, 33, 45, 52, and 58) that it targets. It also prevents most genital warts.
Timing of HPV vaccination
Because HPV is transmitted sexually, the HPV vaccine offers the most protection when given before a person becomes sexually active. Those who are already sexually active may get less benefit from the vaccine. This is because sexually active people may have been exposed to some of the HPV types targeted by the vaccine.
The Centers for Disease Control and Prevention recommends routine HPV vaccination for girls and boys at age 11 or 12 years, and the series can be started at age 9 years. For young people who weren’t vaccinated within the age recommendations, HPV vaccination is recommended up to age 26 years. Some adults between the ages of 27 and 45 years who are not already vaccinated may decide to get the HPV vaccine after talking with their doctor about their risk of new HPV infections.
Children who start the vaccine series before age 15 need two doses to be protected. Those who receive their first dose at age 15 or older need three doses to be protected. Learn more about HPV vaccines and how they protect against cervical cancer and other types of cancer.
Cervical cancer screening
Routine cervical cancer screening with HPV tests and Pap tests is also an important way to prevent cervical cancer. These tests can find abnormal cell changes and precancers that can be treated before they turn into cancer. So it is important for people with a cervix to have regular screening tests starting in their early 20s. Learn more about screening with the HPV test and Pap test.
Lack of access to cervical screening and follow-up of abnormal test results can cause certain groups, such as African American, Hispanic, American Indian and Alaskan Native people and those living in rural areas, to bear a disproportionate burden of cervical cancer. Learn about cancer health disparities.
Because HPV vaccination doesn’t protect against all HPV types that can cause cervical cancer, it’s still important to get screened at regular intervals.
Condoms
Condoms, which prevent some sexually transmitted diseases, decrease the risk of HPV transmission. However, they do not completely prevent it. Exposure to HPV is still possible in areas that are not protected by the condom.
Updated: October 13, 2022
Cervical Cancer Causes, Risk Factors, and Prevention was originally published by the National Cancer Institute.